Greening out is a term used to describe the overwhelming and uncomfortable effects that can occur after overconsumption of cannabis, particularly in high doses. This phenomenon is more common with edibles or potent THC concentrates, as they introduce significant amounts of tetrahydrocannabinol (THC), the psychoactive compound in cannabis, into the body. Here’s a closer look at the causes of greening out, its symptoms, and how to handle it safely.
What Causes Greening Out?
Greening out typically happens when a person consumes too much cannabis, resulting in an overloading of the endocannabinoid system. This system, which regulates various physiological processes such as mood, appetite, and pain perception, can become overwhelmed when exposed to high levels of THC, especially if the person’s tolerance level is low.
This experience is often more intense with edibles because the body metabolizes them differently compared to smoking weed. Edibles release THC slowly over time, which can lead to delayed effects and potential overconsumption when users take more, believing they haven’t consumed enough.
Common Symptoms of Greening Out
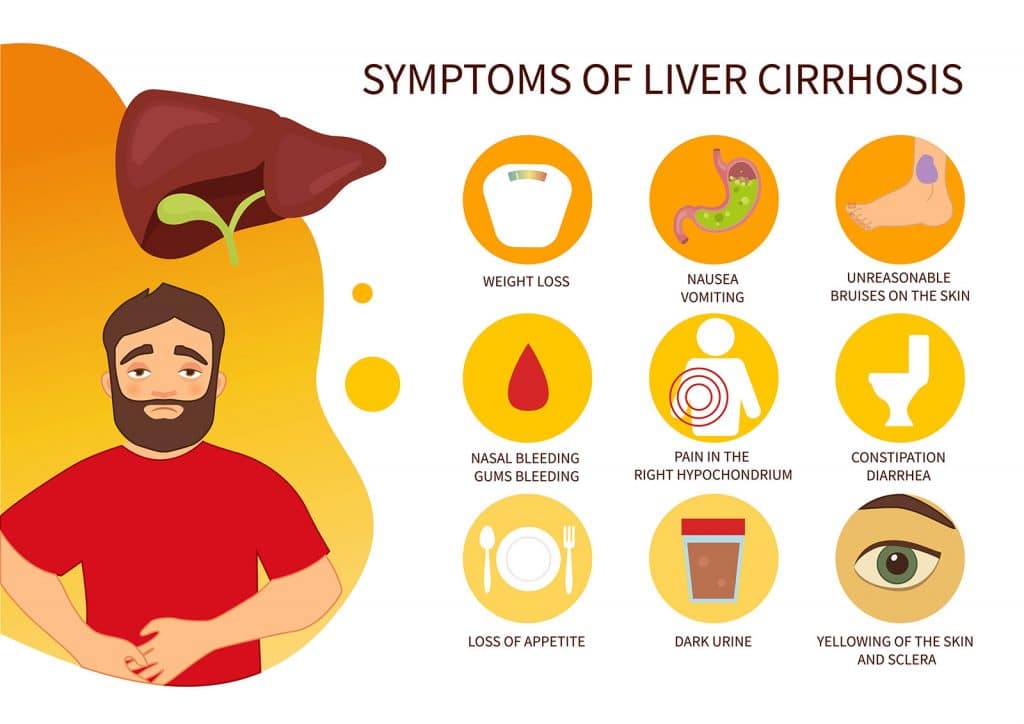
The side effects of greening out can vary depending on the individual, the type of cannabis used, and the amount consumed. Some of the most common greening-out symptoms include:
- Dizziness or lightheadedness
- Nausea or vomiting
- Rapid heart rate (increased heart rate)
- Disorientation or confusion
- Panic attacks or intense anxiety
- Low blood pressure or fainting
- Chills or sweating
These physical symptoms and psychological effects can be distressing but are rarely life-threatening. However, individuals with pre-existing health conditions, especially related to the heart or mental health, should seek medical attention if the symptoms persist or worsen. Proper hydration can help ease some of the discomfort, as dehydration can exacerbate these symptoms.
In some cases, overconsumption of cannabis can lead to cannabinoid hyperemesis syndrome (CHS), a condition marked by severe nausea and vomiting. While CBD (a non-psychoactive cannabinoid) may help mitigate some of the psychoactive effects of THC, it’s important to monitor your consumption to avoid overwhelming the body’s endocannabinoid system.
Why Does It Happen More Often with Edibles and Concentrates?
Edibles and cannabis concentrates contain much higher THC levels than typical marijuana use through smoking. With edibles, the effects of THC take longer to set in because the body must metabolize them through the liver, often leading to delayed psychoactive effects. As a result, users may consume more, thinking the initial dose was insufficient, leading to overconsumption and greening out.
Concentrates, which include products like oils and dabs, also pack a much more potent THC punch, increasing the risk of experiencing adverse effects if used in large amounts or by those with lower tolerance levels.
Managing Greening Out
If you or a loved one is greening out, there are a few steps you can take to ease the symptoms and promote recovery:
- Drink water: Staying hydrated can help mitigate feelings of nausea and dry mouth, common symptoms of greening out.
- Find a safe space: Calm the person by moving them to a quiet, comfortable space where they can take deep breaths and relax.
- Deep breaths: Encourage slow, deep breathing to help manage rapid heart rate and panic attacks.
- Eat something sweet: Low blood sugar levels can contribute to feelings of lightheadedness, so eating a small snack may help stabilize this.
- Rest and recovery: Resting in a calm environment can alleviate some of the disorienting psychological symptoms.
When to Seek Medical Attention
While greening out is rarely dangerous, certain cases may require professional medical help. If symptoms like a rapid heart rate, severe panic attacks, or fainting persist for an extended period, seeking medical attention is advisable. This is particularly true for cannabis users who have underlying heart conditions, mental health disorders, or are using cannabis products in combination with too much alcohol.
Long-Term Considerations: Addressing Cannabis Use and Abuse
For some individuals, greening out may be a one-time event triggered by overconsumption. However, frequent or problematic cannabis use can lead to more serious issues, such as cannabis use disorder (CUD) or substance use disorders. People experiencing frequent adverse effects from marijuana use may want to explore treatment options, including outpatient detox programs or behavioral health interventions, especially if their cannabis use is affecting their well-being.
Treatment Programs for Cannabis Overuse
At Long Island Treatment Center, we offer a range of programs tailored to individuals struggling with marijuana abuse or substance use disorders. Our detox programs, addiction treatment options, and outpatient behavioral health services provide comprehensive care for those dealing with the adverse effects of cannabis use, including those who frequently experience greening out. Our aim is to help individuals regain control over their substance use, improve their mental and physical health, and lead a balanced life.
If you or a loved one is struggling with the effects of cannabis overconsumption or addiction, contact us to learn more about how our treatment center can help you achieve lasting recovery.